ANZUP at ESMO 2025 – ENZARAD
ENZARAD
Name of Trial
ENZARAD: Randomised phase 3 trial of androgen deprivation therapy (ADT) with radiation therapy with or without enzalutamide for high risk, clinically localised, and locally advanced prostate cancer.
Lay Title
ENZARAD: Treatment of prostate cancer that has not yet spread, with radiation therapy and reduction of testosterone, with or without enzalutamide.
Background
Prostate cancer is the one of the most commonly diagnosed cancer in Australians, with more than 28,000 Australian’s expected to be diagnosed with the disease each year. In early-stage disease, where the prostate cancer is confined to the prostate, it is often treated with radiotherapy or surgery, but some people can still have their cancer return (recurrence) or spread to other parts of the body. The ENZARAD trial aimed to optimise outcomes for people affected by local and locally advanced prostate cancer.
What was the trial about?
The ENZARAD trial (ANZUP 1303) was an international, Australian-led study aiming to test whether adding a hormone treatment called enzalutamide to radiation plus testosterone suppression could improve outcomes for people with prostate cancer that is confined to the prostate or nearby tissues, but at high risk of spreading elsewhere. All participants received the best quality radiotherapy treatment (treatment with powerful X-rays to kill cancer cells) together with treatment to reduce the levels of male sex hormones like testosterone that the prostate cancer relies upon for its growth (called androgen deprivation therapy or ADT).
Participants were then randomly allocated to receive treatment with a standard older drug that blocks the effects of the remaining low levels of testosterone or enzalutamide, a newer drug that further blocks the effect of male hormones (androgens) in the body. Nobody on ENZARAD received placebo (inactive) treatment.
Who took part in the trial?
ENZARAD enrolled 802 participants between 2014 and 2018, across 69 hospitals in eight countries including Australia, New Zealand, UK, Ireland, USA, Belgium, Spain, Austria, and Slovenia. About two-thirds of participants were from Australia and New Zealand.
How was the effect of treatment measured?
The main goal was to assess metastasis-free survival (MFS), which is the time from commencement of treatment until the cancer shows up somewhere else in the body, or the patient dies of something else first.
Researchers also looked at:
- How long it took before signs of the cancer came back (progression-free survival)
- How long participants lived overall (overall survival)
- Side effects, to assess the safety and tolerability of enzalutamide in combination with the best standard of care.
Participants were followed for an average of 8 years.
What did the ENZARAD trial find?
Most people participating in ENZARAD had excellent outcomes, and in fact better than we had anticipated when we designed the trial. For most people with cancer localised to the prostate or spread to local lymph nodes, adding enzalutamide to standard treatment did not further improve how long they lived without their cancer spreading.
About 80% of participants were alive at 8 years, regardless of whether they received enzalutamide or not. Most of the deaths that occurred were not due to prostate cancer or to treatment. The addition of enzalutamide did not significantly improve metastasis-free or overall survival for the group, meaning that there is no need to intensify therapy for most people with localised or locally advanced prostate cancer.
However, there was evidence of benefit with the addition of enzalutamide for some people either known to have cancer beyond but close to the prostate (in pelvic lymph nodes), and in those people who received radiation to the pelvic lymph nodes as well as their prostate based on their clinician’s decision.
What were the side effects of treatment?
Most participants experienced mild or moderate side effects typical of ADT therapy and radiotherapy, such as:
- Fatigue (tiredness)
- Hot flushes
More serious side effects were uncommon and occurred at similar rates in both groups, though some (such as high blood pressure and tiredness) were slightly more common in those who received enzalutamide.
What does this mean for trial patients?
The ENZARAD trial helps determine ‘the right treatment for the right patient’ and is a significant step forward in identifying who benefits most from intensified treatment, and also who might not need intensified treatment. This will help doctors and patients decide upon more precise, effective care tailored to each patient’s needs while also avoiding unnecessary side effects from overtreatment. Ongoing research is needed to more accurately identify the patients who benefit from intensification of therapy.
How will the results help patients and doctors in the future?
These results provide confidence to both doctors and patients that for most patients, it is not necessary to add enzalutamide to standard treatment with radiotherapy and ADT. For those at highest risk of spread or recurrence, however enzalutamide may improve outcomes, but further research is needed in this area.
What will the researchers do next?
While the primary purpose of the ENZARAD trial itself is now complete, the team collected tissue samples from participants as well as have the rich clinical data to interrogate. These are being analysed to identify clinical features and biomarkers features in the cancer cells, that might predict who benefits most from intensified treatment with enzalutamide. This work will help guide more personalised care in future.
Further information
ENZARAD (ANZUP 1303) was led by the Australian and New Zealand Urogenital and Prostate Cancer Trials Group (ANZUP) in collaboration with the NHMRC Clinical Trials Centre at the University of Sydney.
The trial received support from Astellas Pharma Inc, and the Prostate Cancer Foundation of Australia.
Poster presentation at ESMO 2025

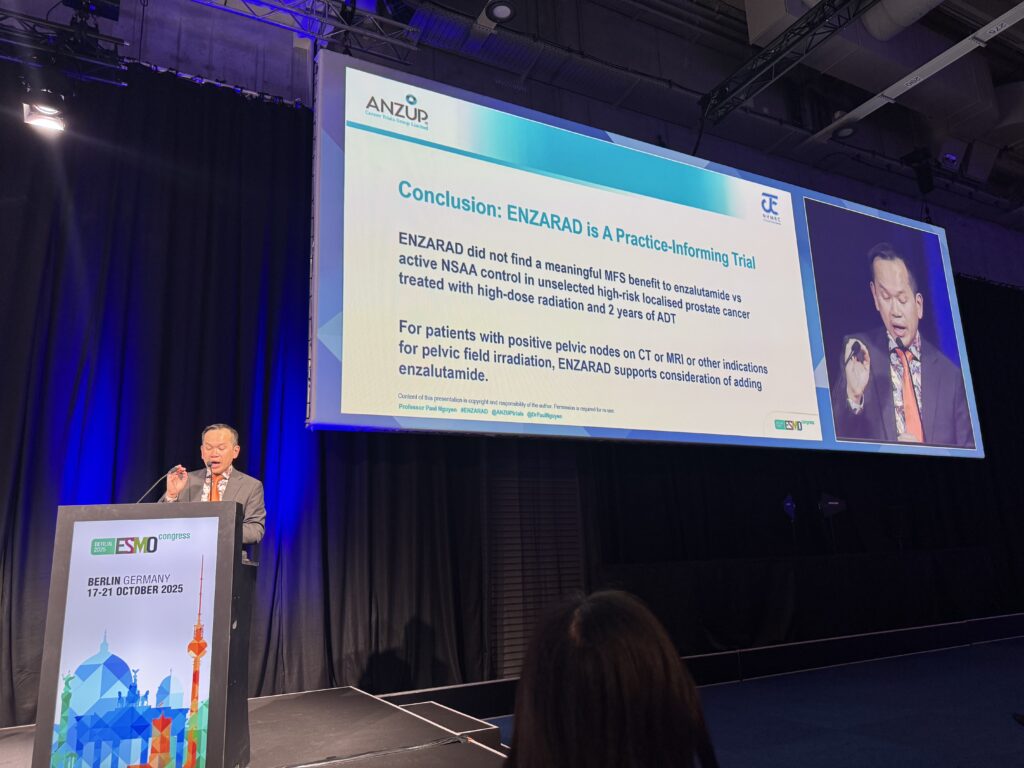
ENZARAD (ANZUP 1303) – Randomised phase 3 trial of androgen deprivation therapy (ADT) with radiation therapy with or without enzalutamide for high-risk, clinically localised prostate cancer. – Presented by Paul Nguyen
The findings provide strong evidence that for most patients it is not necessary to intensify therapy by adding the androgen receptor inhibitor, enzalutamide, to the standard of care (top quality radiotherapy with ADT).
Additionally, in a pre-planned subgroup analysis, ENZARAD showed that for people with the highest risk of recurrence or spread from their prostate cancer (i.e were clinically lymph node positive or those who were planned for pelvic radiation), addition of enzalutamide significantly improved metastasis-free survival defined as the time from randomisation to date of metastasis or death from any cause. These results are practice-informing with positive implications for patients guiding intensification in specific higher risk scenarios.
Prof Nick James, the discussant for the session, described ENZARAD ‘as a very important trial which defines a left hand end to benefit’ [sic] for androgen receptor pathway inhibitors and are consistent with the results seen in the STAMPEDE clinical trial.
Where can I find out more about the trial?
The results will be submitted for publication in a peer reviewed journal and will be available on: https://anzup.org.au/clinical-trial/enzarad-trial/
Trial registration
https://www.clinicaltrials.gov/study/NCT02446444?tab=history
NCT02446444
